What is Skin Cancer?
Skin cancer is an abnormal growth of skin cells, most often caused by exposure to ultraviolet (UV) radiation from the sun or tanning beds. It is the most common type of cancer worldwide, with millions of cases diagnosed each year. Skin cancer comes in several forms, with different levels of severity. The three most common types are basal cell carcinoma, squamous cell carcinoma, and melanoma.
Skin cancer can affect anyone, but certain factors increase the risk, such as fair skin, excessive sun exposure, and a family history of the disease. Early detection and treatment are key to reducing the risk of serious complications.
Who Is at Higher Risk for Skin Cancer?
Skin cancer can develop in anyone, regardless of age, gender, or skin type. However, some people are at higher risk due to various factors such as:
People with fair skin, light hair, and light-colored eyes are more susceptible because they have less melanin, the pigment that protects the skin from harmful UV rays.
Frequent or severe sunburns, especially during childhood, increase the likelihood of developing skin cancer later in life.
Excessive exposure to ultraviolet radiation raises the risk significantly, whether from the sun or tanning beds.
Having many moles or abnormal moles increases the chance of melanoma.
Those with a family history of skin cancer, especially melanoma, are at higher risk.
People with weakened immune systems, such as organ transplant recipients or those with chronic illnesses, are more likely to develop skin cancer.
The risk of skin cancer increases as you age, although younger people can also be affected, especially with prolonged sun exposure.
Remember, even if you don’t fall into these high-risk categories, skin cancer can still affect you! Protecting your skin and performing regular checks is essential for everyone.
Types of Skin Cancer
Skin cancer is the most common form of cancer and is primarily categorized into melanoma and non-melanoma types. Non-melanoma skin cancers are more prevalent and less aggressive, whereas melanoma is less common but more dangerous. Additionally, there are precancerous conditions like actinic keratosis that require attention to prevent progression to cancer.
-
Basal Cell Carcinoma
-
Squamous Cell Carcinoma
-
Melanoma
Basal Cell Carcinoma (BCC)
Basal cell carcinoma (BCC) is the most common form of skin cancer, accounting for about 80% of all cases. It arises from the basal cells in the lower part of the epidermis. While it rarely spreads to other body parts, it can cause significant local damage if left untreated. There are several subtypes of BCC, each with unique characteristics.
Types of Basal Cell Carcinoma
Nodular Basal Cell Carcinoma
This is the most common subtype, typically appearing as a shiny, pearly nodule or bump. It can have visible blood vessels (telangiectasia) and may form an ulcer at the center as it grows.
Nodular basal cell carcinoma is frequently found on the face, particularly the nose, but can develop anywhere on the body.
Pigmented Basal Cell Carcinoma
Pigmented BCC looks similar to nodular BCC but contains darker areas of pigmentation, resembling a melanoma. The pigmentation can range from brown to black.
Pigmented basal cell carcinoma is more common in individuals with darker skin and tends to appear on the face or back.
Morphoeic Basal Cell Carcinoma
This subtype is more aggressive and appears as a firm, scar-like area with ill-defined borders. It often infiltrates deeper into the skin, making it harder to detect.
Typically found on the face and neck, it requires more extensive treatment due to its infiltrative nature.
Superficial Basal Cell Carcinoma
Superficial BCC appears as a red, scaly patch or plaque, often mistaken for eczema or psoriasis. It is the least aggressive type and tends to grow slowly. It is often found on the trunk and limbs, particularly in younger individuals.
How is Basal Cell Carcinoma Treated?
Basal cell carcinoma is treated primarily through surgical removal, such as Mohs surgery. In some cases, topical medications or radiation therapy may be used.
How Can I Prevent Basal Cell Carcinoma?
Protect your skin by avoiding the sun during peak hours (10 AM—4 PM), wearing protective clothing, and using broad-spectrum sunscreen with SPF 30 or higher. Also, avoid tanning beds, as they can also damage the skin.
Squamous Cell Carcinoma (SCC)
Squamous cell carcinoma is the second most common type of skin cancer. It develops in the squamous cells, which are in the upper layers of the skin. SCC is more likely to spread to other parts of the body than BCC, but it’s still highly treatable when detected early. mage Credit: Peter Mullineux / Shutterstock
Subtypes of Squamous Cell Carcinoma
Keratoacanthoma is a fast-growing, dome-shaped skin growth that often appears on sun-exposed areas like the face and arms. It closely resembles squamous cell carcinoma (SCC), making early treatment important to prevent potential complications. While keratoacanthomas may sometimes shrink and disappear independently, they are usually treated as a type of SCC due to their rapid growth and destructive potential.
What does Keratoacanthoma look like?
Typically, keratoacanthoma presents as a firm, round nodule with a central keratin core that resembles a small crater. The growth can reach 1-2 cm in just a few weeks.
What groups have increased chances of developing Keratoacanthoma?
It is most common in people over 60 with significant sun exposure. It’s also more likely in those with weakened immune systems or genetic conditions like Muir-Torre syndrome.
How is Keratoacanthoma treated?
Surgical removal is typically recommended to ensure the growth doesn’t invade nearby tissue or progress to full squamous cell carcinoma. If left untreated, keratoacanthomas can cause scarring, tissue damage, or ulceration, so early detection and treatment are key.
A cutaneous horn is a rare skin growth that appears as a hard, horn-like projection made of keratin, emerging from a red or irritated base. While the horn itself is harmless, the underlying tissue can be benign, precancerous, or malignant, often linked to squamous cell carcinoma (SCC).
What do cutaneous horns look like?
Cutaneous horns are hard, keratinized growths resembling small horns, usually emerging from a red or inflamed base. They can vary in size and shape, with the base potentially benign or cancerous.
What groups have increased chances of developing cutaneous horns?
People with significant sun damage or chronic skin irritation are more likely to develop cutaneous horns. Older adults and those with a history of precancerous skin lesions are at higher risk.
How are cutaneous horns treated?
Surgical removal is typically recommended to examine the underlying tissue for cancer and to ensure proper treatment.
Intraepidermal Squamous Cell Carcinoma (Bowen’s Disease)
Intraepidermal squamous cell carcinoma (SCC), also referred to as Bowen’s disease, is a non-invasive skin cancer confined to the epidermis. While it is a superficial form of squamous cell carcinoma, it can develop into more serious conditions if left untreated. It’s most often caused by long-term exposure to ultraviolet (UV) light and is typically found in areas of the skin exposed to the sun. Early detection is key to preventing progression into invasive SCC.
What does Intraepidermal Squamous Cell Carcinoma look like?
Intraepidermal squamous cell carcinoma typically appears as red, scaly patches or plaques that may turn brown over time. These lesions often grow slowly and can reach several centimeters in size. They are commonly found on sun-exposed areas such as the face, neck, hands, and lower legs.
What groups have increased chances of developing Intraepidermal Squamous Cell Carcinoma?
People with prolonged sun exposure, human papillomavirus (HPV) infection, or weakened immune systems, such as those with HIV or organ transplants, are at higher risk. The condition is also more prevalent in older adults.
How is Intraepidermal Squamous Cell Carcinoma treated?
Treatment options include surgical excision, cryotherapy (freezing the lesion), and topical treatments like 5-fluorouracil or imiquimod, which are applied to the affected area to destroy cancer cells.
How is Squamous Cell Carcinoma Treated?
Treatment usually involves excisional surgery or curettage and electrodesiccation (scraping and burning). In more advanced cases, radiation therapy or chemotherapy may be necessary.
How Can I Prevent Squamous Cell Carcinoma?
Like BCC, prevention of SCC focuses on sun protection, regular skin checks, and avoiding tanning beds. Additionally, individuals with a history of actinic keratosis (a precancerous condition) should be vigilant.
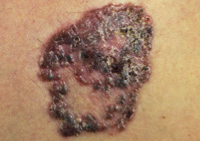
Melanoma
Melanoma is a serious form of skin cancer that starts in melanocytes, the cells responsible for skin pigmentation. While less common than other skin cancers, it is more dangerous because of its potential to spread to other parts of the body. Melanoma can develop from existing moles or as new growths. Early detection is vital for successful treatment.
Signs of Melanoma
Changes in mole size, color, or shape
New dark spots or growths
Moles that bleed, itch, or evolve
Melanoma Risk Factors and Who Is Most at Risk
Melanoma is more likely to develop in certain groups of people due to various risk factors. Understanding these risks can help you take steps to protect your skin and catch any changes early. Check out our list of the most common risk factors that can increase your chances of developing melanoma.
- Sun & Tanning Beds: Frequent exposure to UV rays, whether from the sun or tanning beds, increases your risk.
- Fair Skin: People with lighter skin, freckles, or light-colored eyes have less protection from harmful UV rays.
- Family History: If melanoma runs in your family, you may have a higher chance of developing it.
- Moles: Having many moles or ones that look unusual can be a sign to watch for.
- Weakened Immune System: A weakened immune system can make you more vulnerable.
- Severe Sunburns: Getting severe sunburns, especially in childhood, raises your risk later in life.
- Location: Living near the equator or at high altitudes means more UV exposure.
The ABCDEs of Melanoma
Early detection of melanoma can save lives. The ABCDE rule is a simple way to spot warning signs of melanoma on your skin. Checking your skin regularly using the ABCDE method can help catch melanoma early and lead to better treatment outcomes. If you notice any of these changes, consult a dermatologist right away.
Asymmetry
One half of the mole doesn’t match the other in shape or size.
Border
The edges are irregular, blurred, or jagged.
Color
Look for multiple colors or uneven shading, including black, brown, tan, red, or even blue.
Diameter
Melanomas are typically larger than 6mm (about the size of a pencil eraser), but smaller moles can also be dangerous.
Evolving
Any mole that changes in size, shape, or color or begins to itch or bleed over time needs attention.
Stages of Melanoma
Melanoma is classified into different stages based on its thickness, whether it has spread (metastasized), and the depth of penetration into the skin.
In this early stage, also referred to as In Situ, melanoma is confined to the epidermis (outer layer of skin) and hasn't spread. This is the earliest and most treatable form.
Melanoma has penetrated deeper into the skin, becoming thicker. While still localized, it may have features like ulceration. The tumor has not yet spread to lymph nodes or distant areas.
The melanoma has spread to nearby lymph nodes or skin. Treatment becomes more complex and may involve surgery, immunotherapy, or radiation.
The most advanced stage, melanoma has spread to distant organs such as the lungs, liver, brain, or bones. Treatment focuses on managing the disease with therapies like immunotherapy or targeted drugs.
Types of Melanoma
There are several types of melanoma, each with unique characteristics and patterns of growth. Recognizing the symptoms and understanding the differences between these types can help with early detection and improve treatment outcomes. Below are the main types of melanoma you should be aware of.
Superficial Spreading Melanoma
It is the most common type of melanoma, accounting for about 70% of cases. It grows slowly across the skin before becoming invasive and often presents as flat or slightly raised lesions with irregular borders.
Nodular Melanoma
This type of melanoma is more aggressive and comprises about 15% of melanomas. It penetrates the skin quickly and appears as a dark, dome-shaped growth.
Acral-Lentiginous Melanoma
Acral-lentiginous melanomas are often found on palms, soles, or under the nails. This type of melanoma is common in darker-skinned individuals and progresses rapidly.
Lentigo Maligna Melanoma
Typically associated with long-term sun exposure, this melanoma develops slowly over several years in sun-exposed areas and is more often found in older adults.
Amelanotic Melanoma
This rare melanoma lacks pigmentation, making it harder to identify, although it still exhibits the same growth patterns as other melanomas.
Desmoplastic Melanoma
A rare and aggressive form of melanoma, it is usually found on the head and neck of older individuals. This melanoma often lacks pigmentation which can make diagnosis more challenging.
Information adapted from the National Cancer Institute
How Can I Prevent Melanoma?
While melanoma cannot be entirely prevented, reducing risk is possible by:
- Use a broad-spectrum sunscreen with an SPF of 30 or higher daily, even on cloudy days.
- Wear protective clothing like long sleeves, wide-brimmed hats, and sunglasses.
- Avoid peak sun hours, typically between 10 AM and 4 PM.
- Avoid tanning beds entirely, as they increase the risk of melanoma.
- Schedule regular self-checks and yearly dermatologist visits for professional skin exams
How often should you check your skin?
Most professionals recommend a monthly self-exam and annual dermatologist visit.
Can melanoma be cured?
If caught early, melanoma is often treatable. Advanced melanoma may require aggressive treatment but has seen improved survival with newer therapies.
What should I do if I find a suspicious mole?
Schedule an appointment with a dermatologist as soon as possible for an evaluation and possible biopsy.
Skin Cancer Additional Resources
Navigating through a skin cancer diagnosis or wanting to learn more about prevention can be overwhelming. To assist you, we've compiled a selection of comprehensive resources. These guides and websites offer detailed information on various types of skin cancer, treatment options, and preventive measures, helping you to understand and manage your health effectively.
National Comprehensive Cancer Network's Patient Guide
Start on page 8 for a detailed overview of skin cancer and melanoma.
Click Here To View
Memorial Sloan Kettering
A more detailed description and treatment options for Basal Cell Carcinoma
Click Here To View
Skin Cancer Foundation
More information about Actinic Keratosis from the Skin Cancer Foundation
Click Here To View
National Library of Medicine
More information on Squamous Cell Carcinoma can be found at the National Library of Medicine
Click Here To View
In addition to the websites above, we've compiled the following resources from the American Academy of Dermatology Association to help you protect your skin and detect skin cancer early. These guides have valuable information on sun safety, self-examinations, choosing the right sunscreen, and identifying skin changes. Download these helpful graphics to stay informed and proactive about your skin health.
Skin Self-Exams
Early detection of melanoma can significantly improve treatment outcomes. Learn detailed steps for thorough self-exams by downloading this informative guide.
Protect Your Skin
Sun exposure is a major risk factor for skin cancer. Discover additional strategies for effective sun protection by downloading this comprehensive Sun Safety Tips graphic.
Choosing Sunscreen
Selecting the right sunscreen is important for protecting the protection. This infographic has details like which ingredients to look for and other protective measures.
Detect Skin Cancer
Regular self-checks can lead to early detection of skin cancer. This infographic gives helpful examination techniques, signs to watch for, and ways to keep a record of changes.